
Telemedicine: The Future of Digital Healthcare
Remote medicine, also known as telemedicine, has come a long way in recent years – particularly since the Covid-19 pandemic appeared on the world scene. What was previously its main weakness – i.e. the physical distance between patient and doctor – has now become one of its greatest strengths, as social distancing requirements and a general fear of viral infection have led to more and more people embracing its perceived safety and accessibility as a treatment practice.
The current trend toward this innovative modern medical service, however, comes with its own unique challenges, both legal and practical.
An increasingly complex legal environment
Since telemedicine was fairly uncommon in previous decades, there have been few specific laws enacted to govern the practice in Thailand. Yet this lack of regulatory standards does not mean that operators in this sector are free to operate unchecked – quite the opposite. With no comprehensive policy currently in place, a mishmash of laws written for entirely different purposes may give rise to confusion among operators and medical practitioners when implementing the telemedicine services.
To understand the current legal environment, we must first look more closely at what telemedicine involves. Here are some of the most common types of telemedicine now on offer:
- Interactive Medicine – enables patients to consult with medical professionals in real time via electronic devices, and potentially receive in-home visits.
- Store and Forward – allows healthcare providers to forward and share patients’ medical data with other providers in different locations. This process is normally used for inter-professional purposes, where outsourced diagnostics may be needed.
- Remote Patient Monitoring – permits medical professionals to remotely track patients’ health indicators, such as blood pressure or blood sugar levels. IoT-linked devices such as pill boxes, smart watches, and a variety of other biosensor wearables can also be configured to send data to healthcare providers.
A common thread across these functions is the collection, storage, and potential distribution of sensitive patient data. These processes mean that providers must comply with relevant healthcare laws as well as with the rules surrounding data protection.
The laws that such providers must follow are therefore extremely diverse and hard to follow and understand without proper legal expertise. They include laws as old as the Medical Professions Act B.E. 2525 (1982), as well as regulations that were not even written with telemedicine in mind, such as the Electronic Transactions Act B.E. 2544 (2001) and the Personal Data Protection Act B.E. 2562 (2019), although implementation of the latter law has been delayed until next year. Other twentieth century laws, such as the Medical Facilities Act B.E. 2541 (1998) and the Public Health Act B.E. 2535 (1992), currently govern telemedicine in Thailand as it is practiced today.
More recent regulations have also been introduced with telemedicine in mind, as a result of the pandemic. On July 21, 2020, the Thailand Medical Council issued the Notification Regarding the Guidelines in Respect of Telemedicine or an Online Clinic No. 54/2563 (2020). This notification provides general guidelines surrounding telemedicine services, which were later expanded on February 2, 2021 and referred to as the Notification regarding Standards of Service in Respect of Medical Facilities via Telemedicine System B.E. 2564 (2021) (the “2021 Telemedicine Notification”).
This 2021 Telemedicine Notification sets more robust standards for telemedicine services to adhere to, in particular the following seven criteria:
- The telemedicine service must be a service separate from and additional to the healthcare operator’s existing services as registered under the Department of Health Service Support.
- Operators shall ensure that sufficient professional practitioners and staff are on hand at the medical site.
- Operators shall provide adequate telecommunications and IT systems to facilitate communications between service providers and recipients.
- Operators shall follow standardized processes for every step, from registration and ID verification to consultation and services.
- Professional practitioners must comply with all related standards of care under applicable regulations.
- Operators shall inform patients of treatment methods, service procedures, and risks arising from using telemedicine services.
- Operators shall ensure that telecommunications and IT systems are adequately maintained to mitigate possible risks.
It is notable that public hospitals are not subject to the 2021 Telemedicine Notification, thus they are essentially free to operate remote digital healthcare services without obtaining any specific licenses or permits relating to telemedicine from the relevant Thai authorities.
Nevertheless, the consecutive enactments of these official notifications suggests that the Thai government has come to appreciate the importance of a standardized telemedicine policy. As technology improves and methods become more established, future notifications will certainly involve new adjustments and go into much greater detail.
The Thai government’s stated interest in promoting digital healthcare services should be a source of encouragement for current and potential telemedicine providers. By further clarifying the legal boundaries, the government can open the door to more rapid innovation while ensuring that minimum standards of quality are met.
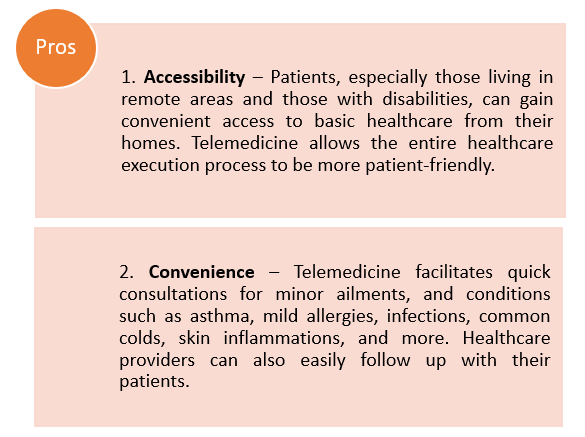
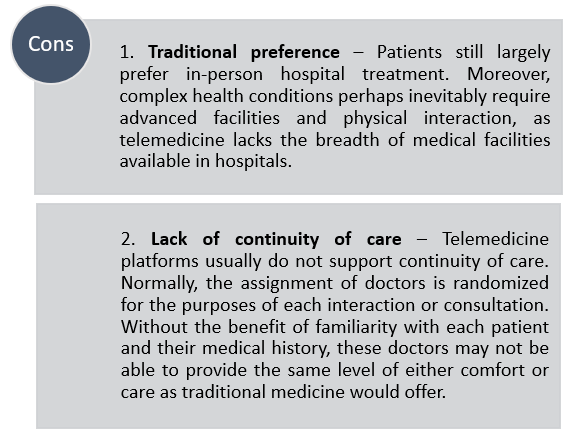
Some pros and cons of telemedicine service
Irrespective of the current pandemic, telemedicine as a service method will always tend to have several distinct advantages and disadvantages. These include:
As medical culture evolves, technology improves, and the industry matures, perhaps this balance will change. Yet with Thai telemedicine and digital healthcare laws still very much in their infancy, the regulatory compliance process is nevertheless complex – and could become more so in the future.
We anticipate the number of patients using telemedicine services will increase due to the social distancing requirements caused by the COVID-19 pandemic as it is a suitable and effective alternative for service providers to communicate with patients. For more information about the relevant regulations or any other notifications relating to telemedicine services, please contact the authors or our team at Kudun and Partners.